Introduction
The World Health Organization (WHO) has issued a stark warning: one in six laboratory-confirmed bacterial infections worldwide is now resistant to standard antibiotic treatment. Financial Times+2Reuters+2 This rising tide of antimicrobial resistance (AMR) is not just a medical issue — it’s a critical health and safety threat at a global scale.
Bacterial infections are becoming one of the leading threats to global health, affecting millions of people every year. These bacterial infections often begin as minor illnesses but can quickly turn life-threatening when antibiotics fail to work. The World Health Organization has repeatedly warned that misuse of antibiotics and poor infection control are fueling this crisis. Without urgent action, routine medical procedures and simple surgeries could become too risky to perform safely.
Across hospitals and communities, bacterial infections are spreading faster than healthcare systems can manage. Many of these bacterial infections now resist multiple types of drugs, forcing doctors to rely on older or less effective treatments. This growing resistance doesn’t just endanger patients — it puts entire populations at risk. Strengthening hygiene practices, vaccination programs, and antibiotic stewardship is critical to slowing the rise of resistant bacterial infections worldwide.
In this article, we unpack what this statistic means, why it matters, and how individuals, institutions, and safety professionals must respond. Why 1 in 6 Bacterial Infections Are Now Untreatable, we see it in detail.
What Does “One in Six” Really Mean?
- The figure comes from a comprehensive WHO report analyzing data from 104 countries between 2016 and 2023. Financial Times+1
- Resistance is rising in about 40% of bacterial samples monitored. Reuters
- In high-risk regions (South Asia, Middle East, parts of Africa), the ratio is even worse — up to one in three infections are drug resistant. Reuters+2The Guardian+2
- The problem is especially severe for Gram-negative bacteria (e.g. Escherichia coli, Klebsiella pneumoniae), which often cause hospital-acquired infections. euronews+2The Guardian+2
In short: what used to be treatable with an antibiotic may now demand more aggressive, riskier, or even experimental therapy — if anything works at all.
Why the Surge in Antibiotic Resistance?
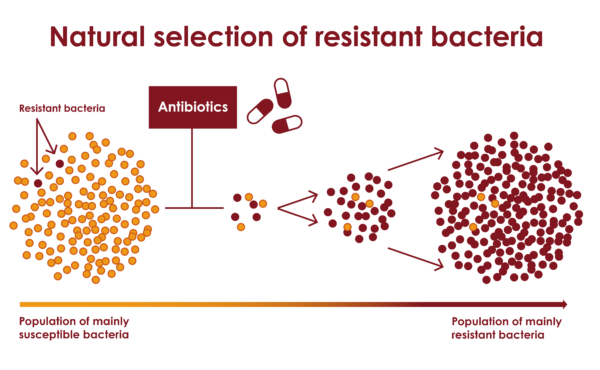
1. Overuse and Misuse of Antibiotics
In many places, antibiotics are easily available (sometimes over the counter), and people take them without prescription, or stop early — giving bacteria opportunity to survive and adapt.
2. Agricultural and Veterinary Use
Antibiotics are used in livestock and farming to promote growth or prevent disease — contributing to environmental spread of resistant strains.
3. Poor Infection Control & Sanitation
Hospitals, clinics, and communities with weak sanitation or infection control can let resistant bacteria spread widely.
4. Lack of New Drugs
The pipeline for new antibiotics and diagnostics is thin. The WHO noted that research and development pipelines are contracting. Financial Times+1
5. Global Inequalities in Access
In places with limited access to diagnostics, patients may receive broad-spectrum antibiotics by default, accelerating resistance.
Health & Safety Implications: Why This Hits Beyond Medicine
Threat to Routine Care
Procedures we take for granted — surgeries, chemotherapy, organ transplants — become riskier when infections can’t be controlled.
Rising Costs & Hospital Burden
Drug-resistant infections usually require longer hospital stays, more expensive treatments, intensive care, and higher mortality.
Workplace & Occupational Risk
Workers in healthcare, agriculture, wastewater treatment, sanitation, and food processing may be exposed to resistant bacteria. Ensuring their safety becomes highly challenging.
Public Safety & Biosecurity
Resistance can spread across borders. A resistant strain emerging in one region can become a global problem, carried by travel or trade.
Key Resistant Bacteria to Watch Why 1 in 6 Bacterial Infections Are Now Untreatable
- Klebsiella pneumoniae — Known for extended-spectrum β-lactamase (ESBL) production and carbapenem resistance. Wikipedia+2The Guardian+2
- Escherichia coli — Common in urinary tract and gastrointestinal infections; many strains now show multidrug resistance. euronews+1
- Acinetobacter baumannii — Known as a hospital “superbug,” increasingly resistant. Wikipedia
- MRSA (Methicillin-resistant Staphylococcus aureus) — A classic example of a bacterial infection slipping from treatable to dangerous. Wikipedia
These bacteria also highlight how health and safety in medical facilities, workplaces, and communities must incorporate resistance control, hygiene, monitoring, and worker protection.
What Can Be Done: A Multi-Layered Response
Clinical & Medical Strategies
- Use rapid diagnostics to identify causative bacteria and resistances before prescribing.
- Tailor antibiotic therapy rather than broad use.
- Monitor dosage and duration carefully to avoid under- or over-treatment (both can promote resistance).
- Encourage development and use of alternative therapies (phage therapy, antimicrobial peptides, etc.).
Public Health & Policy Measures
- Strengthen surveillance systems globally so resistance trends are detected early.
- Regulate antibiotic use in agriculture and veterinary sectors.
- Promote public education on proper antibiotic use.
- Incentivize pharmaceutical R&D for novel antibiotics and diagnostics.
Workplace & Health & Safety (H&S) Actions
- Infectious disease risk assessments in hospitals, labs, agriculture, waste treatment.
- Use personal protective equipment (PPE), strict hygiene, sterilization, and containment protocols.
- Training health personnel and workers on AMR risks.
- Establish guidelines in occupational safety frameworks that include bacterial infection risk as part of safety planning.
Global Coordination
The problem is transnational — no country is safe until all are. Countries must collaborate on data sharing, funding, standardized protocols, and equitable access to medicines.
Outlook and Urgency
If current trends continue, WHO and other researchers warn of major increases in mortality, treatment failures, and health system collapse in vulnerable regions. Financial Times+1 For health and safety, this means we must treat bacterial resistance not just as a medical issue but as a systemic risk — like climate change, pandemics, or industrial hazards.
We are approaching a tipping point. The next decade is crucial to reverse or contain the trend.
Role of OSHAssociation.org in Preventing Bacterial Infections
To help bridge the gap between health and workplace safety, the Occupational Safety and Health Association (OSHAssociation) plays an important role. oshassociation.org+2oshassociation.org+2
At OSHAssociation.org you’ll find:
- Professional certification, training, and standards in Occupational Safety & Health
- Resources and guidance aimed at reducing occupational risks — including those from infectious agents
- A global network connecting safety professionals, researchers, and practitioners
By integrating awareness of bacterial infections and antimicrobial resistance into their frameworks, OSHAssociation helps workplaces adopt preventive measures, manage biological risks, and align safety strategies with emerging health threats.
If you’re writing this article for a journal or platform, consider highlighting how occupational safety bodies (like OSHAssociation) can champion infection control as part of their mandate to protect workers’ health and safety.






